In the first installment of this series, the circumstances which gave rise to my seeing an LLMD were outlined. Having issues getting proper diagnosis and treatment for an early acute case of Lyme disease, the inability to secure a referral to an infectious disease specialist, a referral to a doctor from local Lyme disease support groups, and being incredibly ill all led to my first visit with an LLMD.
In today's installment, I'll talk about how I decided to take antibiotics long term, how the Lyme disease patient community became part of my life, and the inner conflicts which have arisen by being a patient with my condition.
On Being A Somewhat Different Chronic Lyme Disease Patient
Unlike the majority of chronic Lyme disease patients who were surveyed, I did not have to see many doctors before my diagnosis. And unlike the majority of chronic Lyme disease patients, I still felt like modern medicine worked pretty well for me up to that point: If I got bronchitis - the doctor helped. If I got a sinus infection - the doctor helped. If I got an ingrown toenail... You get the idea.
So for me, the health care system - at least up until my Lyme disease experience - worked well enough for me. I received as much care as I needed for the problems I faced and made few demands on the system because I was (for the most part) healthy.
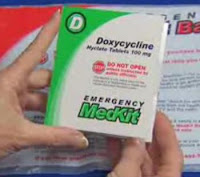
This perspective initially carried over to my LLMD: I thought we would have an appointment or two, I'd check in if I had a question or needed a prescription filled; I'd take antibiotics for a few weeks - and otherwise, our paths probably wouldn't cross again unless I got another EM rash someday.
But as I reached the month mark and realized how lousy I felt, I wasn't so sure about stopping antibiotics. I was severely ill. And when I stopped antibiotics, I discovered that within a few days I was even less functional and in even more pain than I was while taking antibiotics.
I told my LLMD, "I don't understand. I thought I'm supposed to feel better by now. I caught this early." My LLMD said, "This is Lyme. This is how it is."
What do you mean, "This is how it is?"
At that point in the game, my brain was so cognitively impaired I had to take notes and try to reason through this explanation given over time - but to be frank, nothing made sense at that point because I was too ill and wasn't tracking conversations well.
I found out that the choice to continue taking antibiotics rapidly became a pragmatic one:
Every time I stopped taking antibiotics, the worst of my symptoms would return and I would drop out of being an active member of society.
With the antibiotics, I was eventually able to walk up and downstairs at a slow to normal speed. I could drive short distances, I could run some errands, I could walk to the train station, and even begin working part time again. I'd still be in some pain and have some fatigue - but I could at least do something.
Without the antibiotics, I would be overcome with pain and fatigue and begin losing cognitive ground again. I would have trouble leaving the bed - let alone leaving the house. The pain and fatigue were so overwhelming that any stoic attempts on my part to push past them failed.
I didn't like this new reality - but I didn't want to lose my job.
I reasoned to myself that I knew a few diseases were treated with longer courses of antibiotics so there was risk management for such situations - and considered treatment was probably low risk, provided I didn't stop antibiotics and restart them often as that would create antibiotic resistance. Or if I decided to stop and wanted to restart - I could restart with a different antibiotic which was effective in order to avoid resistance.
I rationalized my decision at each step, and I did so directly in response to the improvements I experienced while on antibiotics - but also due to the projected loss if I stopped antibiotics entirely.
I knew the risks to continue the drugs were there - and the risks to stop them were as well. I thought I was damned if I did...and damned if I didn't.
The Ups And Downs Of My New Condition
When I first went off antibiotics and symptoms resurgence occurred, I joined a few online support mailing lists for Lyme disease patients and asked if people knew what was happening to me. I was also in so much pain, I wanted someone else to complain to who would understand and not have to dump on my friends about it.
Outside of Lymeland, my healthy friends knew I contracted Lyme disease - but they could not relate to what I was going through. A few of them had Lyme disease in the past and got it treated - but none of them had developed the kind of problems I had. None of them had symptoms which were as severe as mine or had lasted as long.
It was frustrating, because I didn't understand why my path wasn't the same as theirs. It made me wonder just what was in that tick that bit me that I ended up so much sicker than any of them had been.
Not knowing what else to do, I read the posts and archives on my patient mailing lists and struggled to understand what had happened to me. It was challenging because reading and comprehension came very slowly; I had to take notes because I kept forgetting things.
Before I could understand what was happening to me, a clear picture began to form of what life was like for many patients diagnosed with chronic Lyme disease:
- Most people there had symptoms for a long time before they were given a diagnosis of chronic Lyme;
- Most had already seen multiple doctors who had not been able to diagnosis them - or they were diagnosed with something else but were told their case was "atypical";
- Most felt disowned and dismissed by the medical community at large;
- Most if not all had their lives destroyed in some way by the onset of these symptoms which continued plague them.
Patients who were once married were divorced, due to having partners who were unwilling to be supportive or adapt to the reality of their illness. Patients who lost five and six-figure jobs had to sell their homes and downsize considerably - sometimes moving back in with their elderly parents. Patients who were once avid hunters and rock climbers had to stop doing what they loved and either sold their gear or enshrined it prominently in hopes of using it someday in the far off future.
I didn't know what to make of myself and how I fit into all of this as time went on. It was overwhelming to hear how much physical suffering everyone had endured, how much personal loss everyone experienced, and how much humiliation everyone went through at the hands of various medical professionals.
I swore to myself. This wasn't going to be me. After all, I just had early Lyme disease. Not this chronic stuff. Right?
But as time went on, I realized that as early as my infection had been treated, something wasn't right because like the rest of the group - I was still quite sick.
I was barely able to work part time even with extended treatment. I would get home, take off my shoes, and immediately lie down. I would wait two or three hours before getting up to attempt making myself dinner. And after a simple dinner, I would lie down and pass out for the night.
There was no energy to go out and socialize. It hurt too much to return to clubbing, hiking, and biking. My plan to take surfing classes on Hawaii's beaches was scuttled...There was no money to do it, anyway.
Periodically, I would stop all antibiotics and take painkillers and anti-inflammatory medication instead. But each time, the symptoms which made me totally dysfunctional would come back, and I would give in to taking the antibiotics again and double my consumption of yogurt and acidophilus capsules. Pain medication - over the counter and prescription, both - had little effect on the symptoms I had.
Slowly, very slowly, I improved. Months later, I eventually managed to get a new, full time job - and by the time I did, I was about 80% of my pre-tickbite baseline for health. I was initially relieved and thrilled, because to me this meant I'd finally made it. I thought I'd gotten past the Lyme disease, and wrote off remaining 20% of symptoms as residual fatigue and odd random aches which would heal in time.
This little victory was to be short-lived, however, as after many months of no antibiotics (I had decided to quit, having felt mostly better), I began to relive that sinking sense of decline I'd had the previous year. Cognitive abilities began to wane. Energy lacked. More new symptoms I never had before joined the chorus. I fell behind at work. I attempted to telecommute. But long story short: I had to leave this job, too.
I went to my new family doctor and saw a few specialists and tried to figure out if anything else was going on. We tested for autoimmune disorders - nothing. CBC and metabolic panels - nothing. Vitamin deficiencies? Okay, I was slightly low on B-12, but that was easily correctible.
Nothing else showed up, though. And yet I continued to decline and become increasingly useless. Despondent. Exhausted.
Concerned for my sanity, I decided on my own to consult with a therapist and see if depression or other psychiatric conditions could be causing any of my symptoms. The therapist's evaluation of my situation was that I was somewhat depressed, but the nature and magnitude of my symptoms indicated I had a medical problem that wasn't being properly addressed. What problem? The therapist had no idea.
Not finding any answers from my family doctor, specialists, or therapist, I returned to my LLMD. There, the reason for some of the absolute worst of my symptoms had been revealed: My spiking fevers, sweats, chest compression, and shortness of breath which began attacking at night were pinned down to babesiosis, a tickborne disease caused by babesia - protozoa which cause symptoms similar to malaria. The grinding fatigue and cognitive slowing I'd been struggling with may also have been caused by this organism.
It turned out babesia treatment was the best investment I ever made since the entire Lyme disease debacle began, as it began to alleviate my most serious symptoms. It enabled me to sleep more than three hours a night, restored a huge chunk of my cognitive ability, stopped sharp stabbing pains in my legs, and restored my breathing to normal.
I improved, but to this day have still not returned to my former health before the tick bite.
Trying To Make Sense Of It All
A couple years prior to this point, I went into my situation expecting to take a couple weeks' worth of antibiotics then go back to work. I didn't expect to experience not only a protracted improvement - but also an improvement followed by a more serious decline.
After my cognitive abilities began to improve again, I tried to make sense of my situation: On one hand, clinical trials had shown that only a subset of the most symptomatic patients enrolled improved with additional antibiotic treatment. But on the other hand, I had my own experience with antibiotics over a longer trajectory than those in trials, and had seen greater improvement. On one hand, anecdote is not evidence. On the other hand, I had nothing else to go on because there was no officially sanctioned treatment from the Infectious Disease Society of America, who labeled my condition as being "Post Lyme Disease Syndrome" - hypothesized to be an autoimmune-like disorder.
Tired of having either the contested and hotly debated chronic Lyme disease or the ill-defined Post Lyme Disease Syndrome, I wanted answers. Where were they? Where was the scientific research which would determine my diagnosis without any doubt?
My patient support groups and research I'd read reinforced the idea that Borrelia burgdorferi could cause a persistent infection. But I'd also read that molecular mimicry was associated with Lyme arthritis - at least in some instances. I began to read through all the research I could find, and see if I could independently draw my own conclusions about my condition.
I half jokingly wanted someone to conduct a clinical trial pitting antibiotics against non-antibiotic analogs which contained the anti-inflammatory component. I thought maybe this would answer some questions as to whether it was the anti-inflammatory component of antibiotics which alleviated patients' symptoms - or the antibacterial one. But it was quickly pointed out to me that if any patients were still infected, this would be considered an unethical trial if those patients were placed in the analog arm. I dropped that idea.
I had looked to enroll in clinical treatment trials for either chronic Lyme disease or Post Lyme Disease Syndrome, willing to bet on either horse in this race - but neither was ever running on the NIH-NIAID track whenever I looked. And to this day, there has been no Post Lyme Disease Syndrome treatment trial, and no test of the hypothesis that PLDS - outside of Lyme arthritis - is autoimmune in nature. So my career as a lab rat was over before it could even start.
I wanted to do everything right, and not rely on anecdote alone for my treatment - even if it showed some signs of success. I looked for how I could engage in the research needed to help myself and others - but there was no avenue open for this, either.
So here I was, stuck doing something which I didn't think I'd be doing in the first place and which I wanted to understand: How could I have ended up taking antibiotics longer term when officially published trials indicated that more antibiotics were not better? I thought that as someone with a research background, that I would have used the outcome of those trials as a basis for my decision. I didn't.
One could argue I did it out of desperation. That's probably true. I was so seriously sick, I didn't know what else to do. I was desperate for relief and at one point, nearly suicidal with pain. So desperation played a role - there is no denying that. It was the reality of the situation.
But it really began with the need for a short course of antibiotics to begin with - and ending up continuing it because the alternative was much worse.
And at the time, it was really the only option presented to me by any medical professional outside of pain medicine, and I needed to make sure my brain worked in order to hold down even a part time job - opiates and narcotic pain medicine would have stolen away what brains I had.
I did it because no other options were presented to me, no one else knew how to treat my condition, and the boundaries defining my condition were ill-defined. I definitely had Lyme disease - at least at one point. I definitely had babesia, and now I can never donate blood again. I don't know if any other pathogen was in that tick and will likely never know; perhaps some entirely different microorganism which was antibiotic responsive was killed off by my efforts.
After some time has passed, I've noted that the most severe of my symptoms have not returned. I'm hesitant to say they're permanently gone, given how I was at 80% of my baseline before, only to decline again. And while I'm not well enough to work, I'm not so disabled I can't get out of bed and do a number of basic tasks - provided I pace myself.
Arriving at this stage, I have had to reevaluate how I decide to treat my condition. Since I'm concerned about antibiotic resistance and allergies, I wanted to avoid taking more antibiotics. And since I'm concerned about the condition of my digestive system, I thought stopping antibiotics was in my best interest. So I have stopped again, and tried other methods of treating my symptoms - but none have been effective enough to worth noting.
Today, life goes on - to some degree. I am not improving. I miss working. I miss doing all the things I love to do that I - like so many others on the mailing lists I inhabited - cannot do.
And I debate about what to do next - especially if my symptoms deteriorate more. I am on a rollercoaster where I can't be sure how I'm going to be affected next, and most of the medical community seems ill equipped to know how to manage a patient with my condition.
This is not a blame thing, by the way - this is a simple fact. And yet, if the projections are anything to go by, I am the medical face representing tomorrow's patients: More of us are going to be chronically ill, and have to cope with complex conditions. What can we do to set the groundwork in place to prevent others from becoming chronically ill as I have - and to effectively help those who have become as ill as I am?
(Part three of this series next: The pseudoscience and science of chronic Lyme disease. Part one of this series is here.)

This work by Camp Other is licensed under a Creative Commons
Attribution-NonCommercial-ShareAlike 3.0 Unported License.
Read More In today's installment, I'll talk about how I decided to take antibiotics long term, how the Lyme disease patient community became part of my life, and the inner conflicts which have arisen by being a patient with my condition.
On Being A Somewhat Different Chronic Lyme Disease Patient
Unlike the majority of chronic Lyme disease patients who were surveyed, I did not have to see many doctors before my diagnosis. And unlike the majority of chronic Lyme disease patients, I still felt like modern medicine worked pretty well for me up to that point: If I got bronchitis - the doctor helped. If I got a sinus infection - the doctor helped. If I got an ingrown toenail... You get the idea.
So for me, the health care system - at least up until my Lyme disease experience - worked well enough for me. I received as much care as I needed for the problems I faced and made few demands on the system because I was (for the most part) healthy.
This perspective initially carried over to my LLMD: I thought we would have an appointment or two, I'd check in if I had a question or needed a prescription filled; I'd take antibiotics for a few weeks - and otherwise, our paths probably wouldn't cross again unless I got another EM rash someday.
But as I reached the month mark and realized how lousy I felt, I wasn't so sure about stopping antibiotics. I was severely ill. And when I stopped antibiotics, I discovered that within a few days I was even less functional and in even more pain than I was while taking antibiotics.
I told my LLMD, "I don't understand. I thought I'm supposed to feel better by now. I caught this early." My LLMD said, "This is Lyme. This is how it is."
What do you mean, "This is how it is?"
At that point in the game, my brain was so cognitively impaired I had to take notes and try to reason through this explanation given over time - but to be frank, nothing made sense at that point because I was too ill and wasn't tracking conversations well.
I found out that the choice to continue taking antibiotics rapidly became a pragmatic one:
Every time I stopped taking antibiotics, the worst of my symptoms would return and I would drop out of being an active member of society.
With the antibiotics, I was eventually able to walk up and downstairs at a slow to normal speed. I could drive short distances, I could run some errands, I could walk to the train station, and even begin working part time again. I'd still be in some pain and have some fatigue - but I could at least do something.
Without the antibiotics, I would be overcome with pain and fatigue and begin losing cognitive ground again. I would have trouble leaving the bed - let alone leaving the house. The pain and fatigue were so overwhelming that any stoic attempts on my part to push past them failed.
I didn't like this new reality - but I didn't want to lose my job.
I reasoned to myself that I knew a few diseases were treated with longer courses of antibiotics so there was risk management for such situations - and considered treatment was probably low risk, provided I didn't stop antibiotics and restart them often as that would create antibiotic resistance. Or if I decided to stop and wanted to restart - I could restart with a different antibiotic which was effective in order to avoid resistance.
I rationalized my decision at each step, and I did so directly in response to the improvements I experienced while on antibiotics - but also due to the projected loss if I stopped antibiotics entirely.
I knew the risks to continue the drugs were there - and the risks to stop them were as well. I thought I was damned if I did...and damned if I didn't.
The Ups And Downs Of My New Condition
When I first went off antibiotics and symptoms resurgence occurred, I joined a few online support mailing lists for Lyme disease patients and asked if people knew what was happening to me. I was also in so much pain, I wanted someone else to complain to who would understand and not have to dump on my friends about it.
Outside of Lymeland, my healthy friends knew I contracted Lyme disease - but they could not relate to what I was going through. A few of them had Lyme disease in the past and got it treated - but none of them had developed the kind of problems I had. None of them had symptoms which were as severe as mine or had lasted as long.
It was frustrating, because I didn't understand why my path wasn't the same as theirs. It made me wonder just what was in that tick that bit me that I ended up so much sicker than any of them had been.
Not knowing what else to do, I read the posts and archives on my patient mailing lists and struggled to understand what had happened to me. It was challenging because reading and comprehension came very slowly; I had to take notes because I kept forgetting things.
Before I could understand what was happening to me, a clear picture began to form of what life was like for many patients diagnosed with chronic Lyme disease:
- Most people there had symptoms for a long time before they were given a diagnosis of chronic Lyme;
- Most had already seen multiple doctors who had not been able to diagnosis them - or they were diagnosed with something else but were told their case was "atypical";
- Most felt disowned and dismissed by the medical community at large;
- Most if not all had their lives destroyed in some way by the onset of these symptoms which continued plague them.
Patients who were once married were divorced, due to having partners who were unwilling to be supportive or adapt to the reality of their illness. Patients who lost five and six-figure jobs had to sell their homes and downsize considerably - sometimes moving back in with their elderly parents. Patients who were once avid hunters and rock climbers had to stop doing what they loved and either sold their gear or enshrined it prominently in hopes of using it someday in the far off future.
I didn't know what to make of myself and how I fit into all of this as time went on. It was overwhelming to hear how much physical suffering everyone had endured, how much personal loss everyone experienced, and how much humiliation everyone went through at the hands of various medical professionals.
I swore to myself. This wasn't going to be me. After all, I just had early Lyme disease. Not this chronic stuff. Right?
But as time went on, I realized that as early as my infection had been treated, something wasn't right because like the rest of the group - I was still quite sick.
I was barely able to work part time even with extended treatment. I would get home, take off my shoes, and immediately lie down. I would wait two or three hours before getting up to attempt making myself dinner. And after a simple dinner, I would lie down and pass out for the night.
There was no energy to go out and socialize. It hurt too much to return to clubbing, hiking, and biking. My plan to take surfing classes on Hawaii's beaches was scuttled...There was no money to do it, anyway.
Periodically, I would stop all antibiotics and take painkillers and anti-inflammatory medication instead. But each time, the symptoms which made me totally dysfunctional would come back, and I would give in to taking the antibiotics again and double my consumption of yogurt and acidophilus capsules. Pain medication - over the counter and prescription, both - had little effect on the symptoms I had.
Slowly, very slowly, I improved. Months later, I eventually managed to get a new, full time job - and by the time I did, I was about 80% of my pre-tickbite baseline for health. I was initially relieved and thrilled, because to me this meant I'd finally made it. I thought I'd gotten past the Lyme disease, and wrote off remaining 20% of symptoms as residual fatigue and odd random aches which would heal in time.
This little victory was to be short-lived, however, as after many months of no antibiotics (I had decided to quit, having felt mostly better), I began to relive that sinking sense of decline I'd had the previous year. Cognitive abilities began to wane. Energy lacked. More new symptoms I never had before joined the chorus. I fell behind at work. I attempted to telecommute. But long story short: I had to leave this job, too.
I went to my new family doctor and saw a few specialists and tried to figure out if anything else was going on. We tested for autoimmune disorders - nothing. CBC and metabolic panels - nothing. Vitamin deficiencies? Okay, I was slightly low on B-12, but that was easily correctible.
Nothing else showed up, though. And yet I continued to decline and become increasingly useless. Despondent. Exhausted.
Concerned for my sanity, I decided on my own to consult with a therapist and see if depression or other psychiatric conditions could be causing any of my symptoms. The therapist's evaluation of my situation was that I was somewhat depressed, but the nature and magnitude of my symptoms indicated I had a medical problem that wasn't being properly addressed. What problem? The therapist had no idea.
Not finding any answers from my family doctor, specialists, or therapist, I returned to my LLMD. There, the reason for some of the absolute worst of my symptoms had been revealed: My spiking fevers, sweats, chest compression, and shortness of breath which began attacking at night were pinned down to babesiosis, a tickborne disease caused by babesia - protozoa which cause symptoms similar to malaria. The grinding fatigue and cognitive slowing I'd been struggling with may also have been caused by this organism.
It turned out babesia treatment was the best investment I ever made since the entire Lyme disease debacle began, as it began to alleviate my most serious symptoms. It enabled me to sleep more than three hours a night, restored a huge chunk of my cognitive ability, stopped sharp stabbing pains in my legs, and restored my breathing to normal.
I improved, but to this day have still not returned to my former health before the tick bite.
Trying To Make Sense Of It All
A couple years prior to this point, I went into my situation expecting to take a couple weeks' worth of antibiotics then go back to work. I didn't expect to experience not only a protracted improvement - but also an improvement followed by a more serious decline.
After my cognitive abilities began to improve again, I tried to make sense of my situation: On one hand, clinical trials had shown that only a subset of the most symptomatic patients enrolled improved with additional antibiotic treatment. But on the other hand, I had my own experience with antibiotics over a longer trajectory than those in trials, and had seen greater improvement. On one hand, anecdote is not evidence. On the other hand, I had nothing else to go on because there was no officially sanctioned treatment from the Infectious Disease Society of America, who labeled my condition as being "Post Lyme Disease Syndrome" - hypothesized to be an autoimmune-like disorder.
Tired of having either the contested and hotly debated chronic Lyme disease or the ill-defined Post Lyme Disease Syndrome, I wanted answers. Where were they? Where was the scientific research which would determine my diagnosis without any doubt?
My patient support groups and research I'd read reinforced the idea that Borrelia burgdorferi could cause a persistent infection. But I'd also read that molecular mimicry was associated with Lyme arthritis - at least in some instances. I began to read through all the research I could find, and see if I could independently draw my own conclusions about my condition.
I half jokingly wanted someone to conduct a clinical trial pitting antibiotics against non-antibiotic analogs which contained the anti-inflammatory component. I thought maybe this would answer some questions as to whether it was the anti-inflammatory component of antibiotics which alleviated patients' symptoms - or the antibacterial one. But it was quickly pointed out to me that if any patients were still infected, this would be considered an unethical trial if those patients were placed in the analog arm. I dropped that idea.
I had looked to enroll in clinical treatment trials for either chronic Lyme disease or Post Lyme Disease Syndrome, willing to bet on either horse in this race - but neither was ever running on the NIH-NIAID track whenever I looked. And to this day, there has been no Post Lyme Disease Syndrome treatment trial, and no test of the hypothesis that PLDS - outside of Lyme arthritis - is autoimmune in nature. So my career as a lab rat was over before it could even start.
I wanted to do everything right, and not rely on anecdote alone for my treatment - even if it showed some signs of success. I looked for how I could engage in the research needed to help myself and others - but there was no avenue open for this, either.
So here I was, stuck doing something which I didn't think I'd be doing in the first place and which I wanted to understand: How could I have ended up taking antibiotics longer term when officially published trials indicated that more antibiotics were not better? I thought that as someone with a research background, that I would have used the outcome of those trials as a basis for my decision. I didn't.
One could argue I did it out of desperation. That's probably true. I was so seriously sick, I didn't know what else to do. I was desperate for relief and at one point, nearly suicidal with pain. So desperation played a role - there is no denying that. It was the reality of the situation.
But it really began with the need for a short course of antibiotics to begin with - and ending up continuing it because the alternative was much worse.
And at the time, it was really the only option presented to me by any medical professional outside of pain medicine, and I needed to make sure my brain worked in order to hold down even a part time job - opiates and narcotic pain medicine would have stolen away what brains I had.
I did it because no other options were presented to me, no one else knew how to treat my condition, and the boundaries defining my condition were ill-defined. I definitely had Lyme disease - at least at one point. I definitely had babesia, and now I can never donate blood again. I don't know if any other pathogen was in that tick and will likely never know; perhaps some entirely different microorganism which was antibiotic responsive was killed off by my efforts.
After some time has passed, I've noted that the most severe of my symptoms have not returned. I'm hesitant to say they're permanently gone, given how I was at 80% of my baseline before, only to decline again. And while I'm not well enough to work, I'm not so disabled I can't get out of bed and do a number of basic tasks - provided I pace myself.
Arriving at this stage, I have had to reevaluate how I decide to treat my condition. Since I'm concerned about antibiotic resistance and allergies, I wanted to avoid taking more antibiotics. And since I'm concerned about the condition of my digestive system, I thought stopping antibiotics was in my best interest. So I have stopped again, and tried other methods of treating my symptoms - but none have been effective enough to worth noting.
Today, life goes on - to some degree. I am not improving. I miss working. I miss doing all the things I love to do that I - like so many others on the mailing lists I inhabited - cannot do.
And I debate about what to do next - especially if my symptoms deteriorate more. I am on a rollercoaster where I can't be sure how I'm going to be affected next, and most of the medical community seems ill equipped to know how to manage a patient with my condition.
This is not a blame thing, by the way - this is a simple fact. And yet, if the projections are anything to go by, I am the medical face representing tomorrow's patients: More of us are going to be chronically ill, and have to cope with complex conditions. What can we do to set the groundwork in place to prevent others from becoming chronically ill as I have - and to effectively help those who have become as ill as I am?
(Part three of this series next: The pseudoscience and science of chronic Lyme disease. Part one of this series is here.)

This work by Camp Other is licensed under a Creative Commons
Attribution-NonCommercial-ShareAlike 3.0 Unported License.